UNDERSTANDING THE ANKLE SYNDESMOSIS IN SPORTS-RELATED ACTIVITIES SPECIFICALLY IN LONG DISTANCE RUNNERS & DISCUSSING TYPES OF TREATMENTS APPROACHES
The ankle syndesmosis injury is pathology relatively
common in sport players, but first, what
is the ankle syndesmosis? It’s a fibrous articulation in which
bones, shinbone and fibula, are connected by a fibrous tissue sheet. Thanks to
the ankle syndesmosis we are able to walk, run and play any sport and if it
becomes a problem this could be substantially harmful for our health and a
disability for people’s day-to-day activities. Figures have been published
where it has been pointed out that this kind of condition can reach from 1% up
to 11% of all ankle injuries. (A. Molinari et la, 2009).
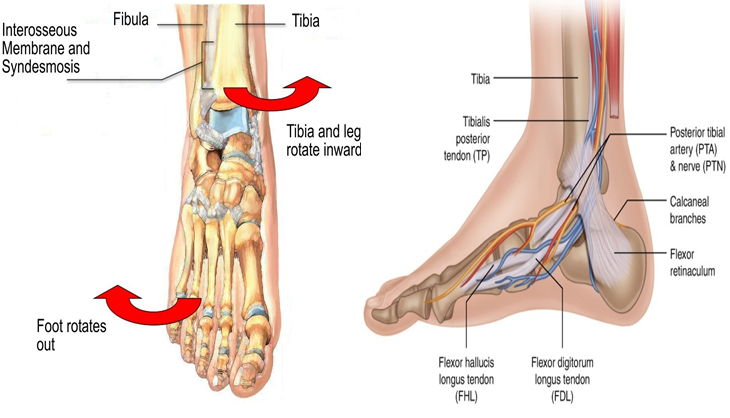
Discussing a little more of ankle´s physiology, shinbone
and fibula make a cupola into which talus fits allowing flexion and extension
movements, between those ones there’re different ligaments that support bones
together prevent from their separation, one example about ligament is
syndesmosis that keep together the most distal part of shinbone and fibula.
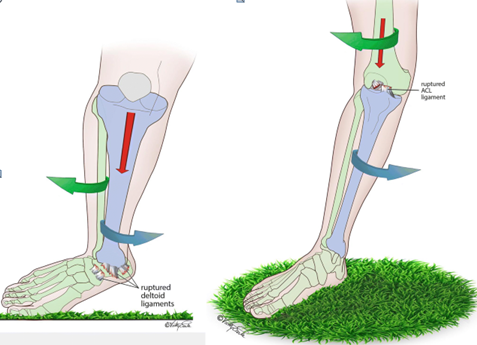
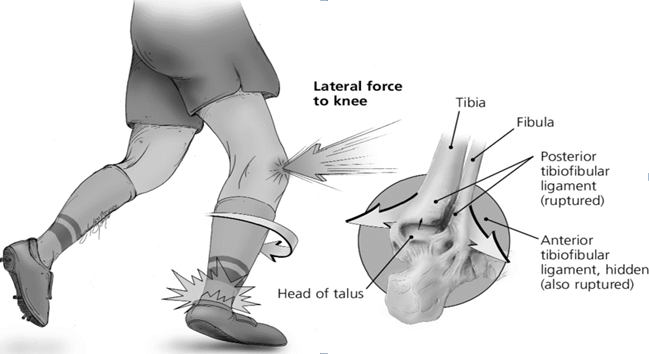
Likewise, syndesmosis ruptures cause a lot of problems and permanent effects about pain and instability that need surgical intervention. This one could happen with several ankle motions, but the most frequent motions are severe external rotation or dorsiflexion of the Talus. On the other hand, talus dome is wider in its anterior part than posterior and these movements make a distance between medial and lateral aspects. It is also paramount to bear in mind that according to literature the timeframe which an athlete will be out of the field due to high ankle sprain also known as ankle syndesmosis can vary from 0 days to 137 days averaging 52 days to complete rehab and return to their prior sporting proficiency in most of the cases. (Jones MH et la, 2007).
SO, WHAT EXACTLY IS THE ANKLE SYNDESMOSIS?
This condition is a sprain of one or more of the ligaments that hold the tibia and fibula together in the ankle. This joint, called the ankle syndesmosis, is made up of ligaments at the front and back of the ankle, and in the space between the tibia and fibula.
In the same way, ankle syndesmosis sprain usually happens to athletes that participate in sports like American football, running, basketball, football or downhill skiing, generally physical activities that need continuous movements of legs, feet and ankles. In as much as, reports have claimed that high ankle sprains can come about at an average of 1 athlete out of 10.000 i.e., its incidence is quite low compared to other of its same kind. Furthermore, it is more likely that this ankle condition occur in male athletes than female ones. (Mauntel TC et la, 2017).

Football injuries usually occur by forced external rotation of the foot while the athlete is prone, it gets together with a fractured ankle. Likewise, a damage of the ankle could happen by a blow to the lateral knee while foot is planted and dorsiflexed, coming in an external rotation moment at the joint.
We have other sports or activities like the downhill ski racing, where because of using boots that make difficult dorsi or plantar-flexion movements, this finally results in excessive external rotation and damage of anterior or posterior ankle ligaments.
HOW CAN HIGH ANKLE SPRAIN BE DIAGNOSED? IS IT NECESSARY IMAGING STUDIES?
First of all, the most important symptom is pain that feels over ligaments anterior and inferior ankle, and over posterior and inferior, found between shinbone and fibula. The ankle syndesmosis injury usually doesn’t become inflamed as another ankle sprain, which give the idea about that it is not a gravely injure but however it presents symptoms like: pain over the ankle being irradiated to leg, pain that become worse while walking, pain about spin around or flex ankle, problems to get up calf muscle and incapacity to support our wight over ankle.
Generally, the symptoms are these ones but it could change between every person, either to be worse or better, this is the reason why it needs a correct and thorough diagnosis. The ankle syndesmosis injury is difficult to diagnose because it doesn't indicate important external symptoms of a grave injury, in addition to knowing what events caused the damage it's crucial to do a correct diagnosis.
Secondly, to do a diagnosis it should do a physical clinical test performed by sports specialist physician or Manchester city physio that includes; squeeze and manipulation of leg and foot to evaluate rotation, flex and support of weight. Next to physical test an x-ray to visualise if there is bone fracture and tomography or magnetic resonance to visualize tears and injuries on ligaments and tendons.
High Incidence
Studies about ankle syndesmosis have proved that it is more frequent in football, rugby, hockey and skiing. A research study was carried out in United States where there were 1821 diagnosed persons with ankle syndesmosis injury and the incidence rate was about 2,09 per 100.000, finally on estimated of 6445 syndesmotic injuries per year. The incidence is lower than other injuries and it's more common in young people.
Another study finished in National Collegiate Athletic Association (NCAA) football players resulted in an incidence of 0,24 /1000 athletes, accounting for about 24,6% of all ankle sprains. Complete syndesmosis injuries resulted in significantly greater time lost compared with partial injuries (Hunt, Kenneth J. MD et la 2012). Finally concluded that there was a higher probability of injury in plays than practices, also were high incidence in cases that occur over artificial than natural grass and the most occur while in contact with another athlete.
Being a sport when run is one of the most important activities, we can say that incidence of ankle syndesmosis injuries in runners is not a lot frequently and it happens by an extreme rotation of ankle when it is flex in a static position, it cloud be because a drop during running or a slip, causing a damage in the syndesmosis and effects over instability and osteoarthritis if it continues in the time without being treated with physiotherapy at My Sports -related injuries Clinic in Manchester City.
PHYSIOTHERAPY TREATMENT AT MY SPORTS INJURY? WHEN IS IT NECESSARY?
Having sustained an Ankle lesion you must be compress, raise the ankle, put ice and take a lot of rest. Next, the treatment depends on characteristics of the ankle condition, if it is a stable or a unstable lesion. Stable lesion of syndesmosis is when there is integrity of medial ligamentous complex (medial ankle side) and the treatment is based on a comprehensive rehabilitation joint discharge model which can last for 3 weeks, also consecutive physiotherapy reviews for exercise progression and proprioception exercises. But however, it can commonly present with complications like rigidity, pain, swelling and repeated sprains. Your Physiotherapist at MY Sports Injury can give you full guidance at your appointment visit.
On the other hand, unstable lesions need surgical treatment to reduce and stabilise structure in their correct position, to get appropriate grafts of ligaments and prevent early secondary degenerative changes. In the case of isolated syndesmosis, they used different fixing methods like static fixation with screw, dynamic fixation, and reconstruction plasties.
Sports Physiotherapy treatment options for this injury can range from rest and ice to surgery, depending on the severity of the injury. It is important to seek professional medical advice from a Physiotherapist if you suspect you have a syndesmosis injury, as prompt treatment can help prevent long-term complications and promote healing.

REFERENCES
Molinari A, Stolley M, Amendola A. High ankle sprains (syndesmotic) in athletes: diagnostic challenges and review of the literature. Iowa Orthop J. 2009;29:130-8. PMID: 19742102; PMCID: PMC2723709.
Jones MH, Amendola A. Syndesmosis sprains of the ankle: a systematic review. Clin Orthop Relat Res. 2007;455:173–5
Mauntel TC, Wikstrom EA, Roos KG, et al. The epidemiology of high ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med 2017;45(9):2156-2163





