UNDERSTANDING THE MEDIAL TIBIAL
STRESS SYNDROME ALSO KNOWN AS TIBIAL PERIOSTITIS & SOLEUS SYNDROME HOW TO
TREAT AND REHAB MEDIAL TIBIAL STRESS SYNDROME BASED ON NON-OPERATIVE MANAGEMENT
& EXERCISES
Have you ever wondered how to straightforwardly
solve your shin splints pains? Read this below, let’s jump right in!
Periostitis is a rather common condition in
athletes, dancers, and military personnel, especially long-distance runners. It
is also known as medial tibial stress syndrome or shin splints; it is deemed as
an aching and benign condition which adds up to an incidence from 4% up to 35%.
(Noam Reshef et la 2012). More concretely 13.6% up to 20% in runners and 35% in
the army.
It cannot be obviated that running is one of the most common and practiced sports across the world. Thus, being this a fact if you get to practice jogging and running in a regular basis this can become detrimental to your lower limbs particularly to your calves, legs, sole foot, ankles, and toes. Running is indeed tied in to pick up your overall health and longevity, nonetheless, is also greatly linked to own a high risk to lower extremities injuries since 50% of the active running practitioners have claimed to sustain more than one injury a year. (M Tschopp et la 2017).

So, how can we describe the Medial Tibial Stress Syndrome, Periostitis, Shin Splints from an anatomical point of view?
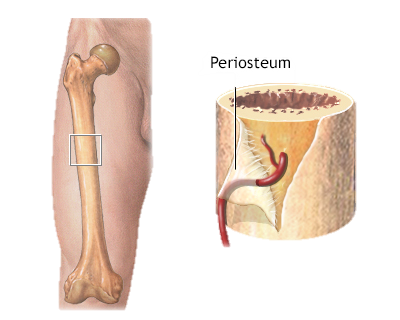
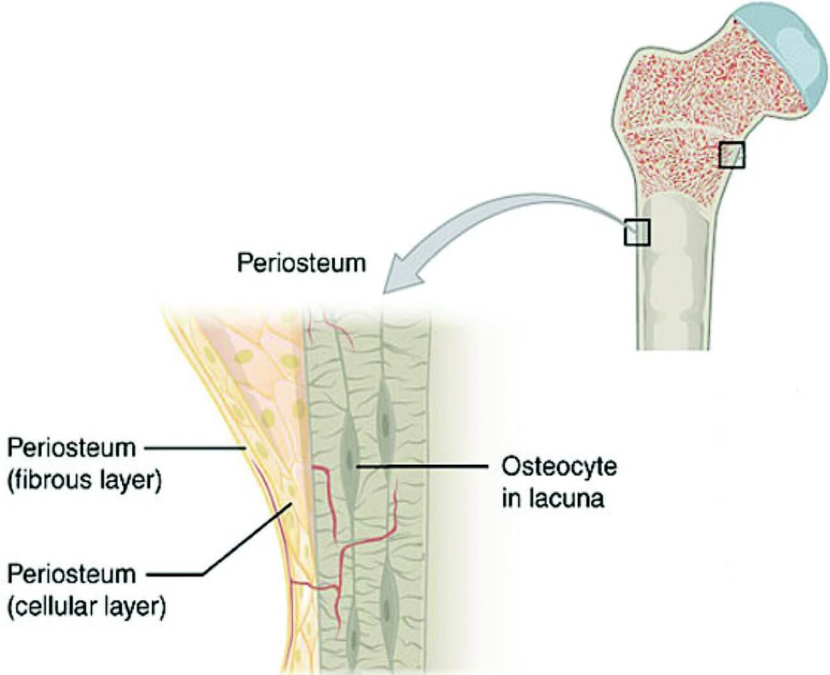
About every bone in the human body is covered by periosteum, however, it has been the focus of debate as it is not comprehended in its full extent. What is clearly known nowadays according to literature is that the periosteum is a membrane that covers the bone and provides it with irrigation, nutrition, and sensitivity. The muscles that reach the tibia are attached to this membrane, so "periostitis" can be caused not only by inflammation of the periosteum, but also of the adjacent muscles and tendons such as the tibialis posterior, tibialis anterior, soleus, and extensors and flexors of the toes. It is included within overuse injuries, as are stress fractures and Achilles tendinopathy. (Jerry R. Dwek 2010).
WHAT CAN BRING ON TIBIAL PERIOSTITIS?
A repeated overload during the race, which overwhelms the body's reparative mechanisms, causes an inflammation of the tissues around the tibia, i.e., it is due to overuse and exercises-induced pain in the anterior tibia area mostly brought on by jumping, long-intense running, and sprinting. (Charles J. McClure et la 2021).
The factors that can cause periostitis are; incorrect training, i.e., a sharp increase in the intensity or duration of physical activity, running on very hard or very uneven surfaces, inadequate or worn shoes.

WHAT ARE THE SYMPTOMS OF TIBIAL PERIOSTITIS?
The typical clinical picture is pain in the anterior aspect of the leg, either internal or external. The clearest symptom of this injury is a pain that appears when starting physical activity and that decreases after a short warm-up period, but that reappears and with more intensity, when running for a while. The runner experiences a sore or burning sensation in the affected area. This pain gradually fades after a few days of rest and reappears when the patient returns to sports activity.
According to research studies claim that a new spectrum of tibial stress injuries is liable to be entailed in the Medial Tibial Stress Syndrome taking in conditions like tendinopathies, stress reaction of the tibia, peroneal remodelling, and periostitis. In addition, there are other dysfunctions involve in this Tibial Periostitis pathology such as the ones which take place over the soleus muscles, and tibialis posterior and tibialis anterior. (R. Michael Galbraith et la 2009).
When the picture becomes more severe, the pain can be permanent and even at rest. It is at this time that the orthopaedists or physios in Manchester should be consulted to rule out a more serious injury such as a stress fracture of the tibia.
HOW IS TIBIAL PERIOSTITIS TREATED CONSERVATIVELY?
In acute stage ice and rest. Rest does not necessarily mean total suspension of physical activities. You can decrease the training load, either distance or frequency. Or switch to cycling or swimming to maintain aerobic capacity. This rest is variable depending on the severity of the symptoms and can range from 2 to 6 weeks. Ice is very useful and can be applied for periods of 20 minutes after physical activity, or several times a day. Anti-inflammatories or paracetamol are also helpful.
Modify training program, decrease intensity, frequency and duration, perform low-impact exercises (elliptical, bicycle, etc.), gradual return to sports activity if there is no pain, perform regular stretching and strengthening of the lower limbs and trunk (glutes, abdominals and hips), suitable shoes for the type of footprint and with shock absorption, change shoes every 400 to 600 km, consider using insoles if necessary, kinesiology and physiotherapy in Manchester (exercises, transcutaneous electrical nerve stimulation, etc.).
The leading treatment includes strengthening and stretching exercises for the Medial Tibial Stress Syndrome which can be guided by our Sports Injury Specialist physiotherapists at My Sports Injury Clinic based in Manchester City.
Sports physiotherapy clinicians, sports massage therapists, and manual therapists are some of our experts in sports-related injuries that will help you to fix Medial Tibial Stress Syndrome pain in Manchester.
We help you go through this situation our sport injury specialists with great expertise, who will address, assess and determine what the most suitable treatment options are for your individual needs, this may vary between sports massage or more complex manual therapy techniques provided in our Manchester City centre location.
At My Sports Injury Clinic Manchester we strive for our patients to be in a healthy optimal state both mentality and physically so providing a series of proven conservative treatments that help alleviate, heal and keep your condition away from exacerbating, there are more structured physical therapy programs including, acupuncture in Manchester, Osteopathic techniques for correction purposes to the joints, Chinese massage & cupping therapy, deep tissue, thermotherapy and sports massages, dry needling, and postural correction rehabilitation amongst others.
HOW LONG DOES IT TAKE TO GED RID OF TIBIAL PERIOSTITIS?
Normally you can be fully recovered in a period of 3-12 weeks, depending on the evolution of your recovery and the time you have the injury, although it could take up to 6 months. On rare occasions it is necessary to apply surgery, where the recovery time will be 3 months.
WHAT ARE THE BEST EXERCISES TO TARGET AND RELIEVE TIBIAL PERIOSTITIS PAIN AND DISCOMFORT?
Shin splints is one of the most common injuries in runners in Manchester. One of the reasons this problem occurs is that strength is not being trained. The good news is that it can be treated and that there are exercises to relieve the pain.
Tibial periostitis is an injury characterized by inflammation of the area that covers the tibia. The main symptom of this problem is constant pain, which can be disabling in some cases. Many runners suffer this injury caused by the continuous impact on the tibia while running, which causes the area to swell and shin splints to appear. It is true that a good running technique helps to prevent it, but this is not always the case, so there are also runners who have a good technique but suffer from these discomforts.
Tiptoe work
Stand up or squat, lift the sole of your foot slowly and hold it up for a few seconds. It's tough and you may feel quite a bit of tension in your calves and shinbone, a cramp-like warmth. But all this is part of the activation and strength gain. It is a very simple exercise, hard but very effective.

Tibial stretch
Get down on your knees and we'll back down. That elongation of the body will depend on your flexibility. Rest your hands close to and behind your buttocks if you want to go slow. The slowness and progression of the exercise is very important, if you force yourself, you could injure yourself and that is exactly the opposite of what is intended.

Strengthening of tibialis with resistances
You can use a rubber with medium resistance, increase the intensity once you feel that it is no longer enough. Sit on the ground and tie both ends to a trellis or any other surface that is well anchored to the wall and won't be able to come off. Insert one foot into that V that the rubber has formed and push the entire sole backwards, as if you wanted to touch your nose but without lifting your leg off the ground. This will have to remain stretched and attached to the ground.

CAN TIBIAL PERIOSTITIS BE PREVENTED?
Periostitis is one of the most frequent overuse conditions in runners. It can be prevented with proper training and appropriate shoes. When it occurs, it is important to reduce the training load and temporarily change it for low-impact activities. When the pain becomes constant or at rest, it is advisable to consult a traumatologist. Proper diagnosis and early treatment will allow for a speedy return to training.
REFERENCES
Reshef N, Guelich DR. Medial tibial stress syndrome. Clin Sports Med. 2012 Apr;31(2):273-90. doi: 10.1016/j.csm.2011.09.008. PMID: 22341017.
Tschopp M, Brunner F. Erkrankungen und Überlastungsschäden an der unteren Extremität bei Langstreckenläufern [Diseases and overuse injuries of the lower extremities in long distance runners]. Z Rheumatol. 2017 Jun;76(5):443-450. German. doi: 10.1007/s00393-017-0276-6. PMID: 28236094.
Dwek JR. The periosteum: what is it, where is it, and what mimics it in its absence? Skeletal Radiol. 2010 Apr;39(4):319-23. doi: 10.1007/s00256-009-0849-9. PMID: 20049593; PMCID: PMC2826636.
McClure CJ, Oh R. Medial Tibial Stress Syndrome. [Updated 2021 Nov 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538479/
Winkelmann ZK, Anderson D, Games KE, Eberman LE. Risk Factors for Medial Tibial Stress Syndrome in Active Individuals: An Evidence-Based Review. J Athl Train. 2016 Dec;51(12):1049-1052. doi: 10.4085/1062-6050-51.12.13. Epub 2016 Nov 11. PMID: 27835043; PMCID: PMC5264561.
Galbraith RM, Lavallee ME. Medial tibial stress syndrome: conservative treatment options. Curr Rev Musculoskelet Med. 2009 Oct 7;2(3):127-33. doi: 10.1007/s12178-009-9055-6. PMID: 19809896; PMCID: PMC2848339.





